Real Reviews From Real Patients
See What Our Patients Are Saying
Live Without Constant Pain
Physical Therapy
Pain and discomfort gets in the way of living life the way you want to live it. Work one-on-one with an expert physical therapist for your whole session. We give you our complete, undivided attention for the best results.
Feel Rejuvenated
Massage Therapy
Experience total relaxation and release the pain from your body during a professional, affordable massage session. Our expert massage therapist listens to you and helps alleviate your aches and pains.
Don't wait weeks
No Wait Times, We Can Schedule You Sooner
Your pain isn't waiting, so you shouldn't have to either.
We have a team of dedicated, experienced Physical Therapists standing by to help. Reach out to our team and get an appointment scheduled as quickly as you can fit it in your schedule.
For those that need more care
PT Effect Advantage Plan
The PT Effect Advantage Plan is a comprehensive annual program that helps you maintain your health and reach new goals. With this plan, we’ll be enabled to treat you outside the limits of insurance. This allows for the complete optimization of your health needs.
The Best Of The Best
Meet the Team
Learn more about the expert physical therapists and team members that you'll work with at our clinic. Every physical therapy session will be one-on-one with a Licensed Doctor of Physical Therapy.

Dr. Mark Shulman
Doctor of Physical Therapy (DPT), Fellow of the American Academy of Orthopaedic Manual Physical Therapists (FAAOMPT), COMT, CSCS
Owner

Dr. Allison McKay
Doctor of Physical Therapy (DPT), Pelvic Rehab Practitioner Certification (PRPC)

Dr. Hannah Willms
Doctor of Physical Therapy (DPT)

Dr. Jana Tokunaga
Doctor of Physical Therapy (DPT)

Dr. Sarah Mendenhall
Doctor of Physical Therapy (DPT)
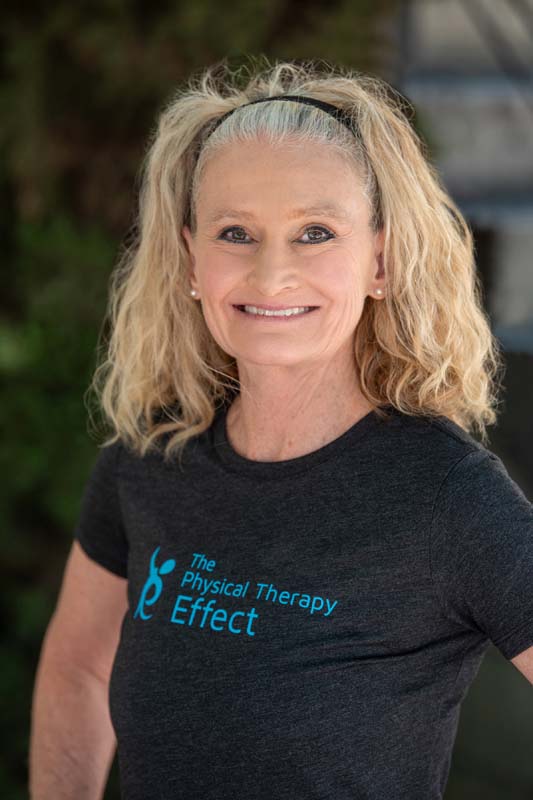
Jil Harris
Personal Trainer

Julissa Amina
Certified Massage Therapist (CMT)

Rachel Berger
Office Manager
Convenient Downtown Location
State-of-the-Art Office
We’ve been a part of the Little Italy community for over 6 years. Our office features top-of-the-line equipment to get you the results you expect.




Manual Therapy
How We Achieve A Better Diagnosis with Less Discomfort
What is manual therapy? Manual therapy is a method physical therapy that involves the therapist feeling exactly how your body reacts to specific movement and exercises. A lot of pain and discomfort comes from lack of mobility or a small range of motion. Through simple movements and exercises, we're able to get your body used to these motions again, reducing or completely removing your pain.
Manual therapy includes a detailed biomechanical assessment. This means that your therapist will watch and feel how you move in order to make the most accurate diagnosis possible. This leads to faster recovery times and improved outcomes.
Benefits of Manual Therapy
More accurate diagnoses and understanding of pain

Less discomfort and pain during treatment
Therapist can feel where there is tension and mobility issues